Femoral hernia
See general information on hernia here.
Anatomy
A femoral hernia is a hernia in the groin area.
It often presents as a small swelling just below the groin crease, and is often mistakenly thought of as a swelling on the inside of the top of the thigh.
It often presents as a small swelling just below the groin crease, and is often mistakenly thought of as a swelling on the inside of the top of the thigh.

It occurs through the femoral canal – a natural occurring canal located between the femoral vein and the pubic bone.

Femoral hernia.
Symptoms and signs
Small to moderate hernias
These hernias are quite often asymptomatic—with no pain or bulge. Because of this, femoral hernias are ‘dangerous’, as they may only become noticeable with strangulation, which is a surgical emergency.
Large hernias
These may present as a bulge in the groin near the upper thigh. There will be discomfort or pain in the groin area. It is also possible to feel some pain in the hip area too.
Strangulated hernia
The patient presents with:
These hernias are quite often asymptomatic—with no pain or bulge. Because of this, femoral hernias are ‘dangerous’, as they may only become noticeable with strangulation, which is a surgical emergency.
Large hernias
These may present as a bulge in the groin near the upper thigh. There will be discomfort or pain in the groin area. It is also possible to feel some pain in the hip area too.
Strangulated hernia
The patient presents with:
- severe groin pain that occurs suddenly
- nausea, vomiting
- abdominal bloating/distention
- a very tender lump may be apparent.
Risk factors for femoral hernia
Female
70 % of femoral hernia occurs in female. This is probably due to the larger female pelvis, hence a larger femoral canal.
Middle age
Chronic straining of the abdominal muscles causing a weakening of the muscular wall. Factors that can precipitate chronic abdominal wall straining include:
70 % of femoral hernia occurs in female. This is probably due to the larger female pelvis, hence a larger femoral canal.
Middle age
Chronic straining of the abdominal muscles causing a weakening of the muscular wall. Factors that can precipitate chronic abdominal wall straining include:
- obesity
- pregnancy
- repeated heavy lifting
- chronic coughing.
Femoral hernia repairs
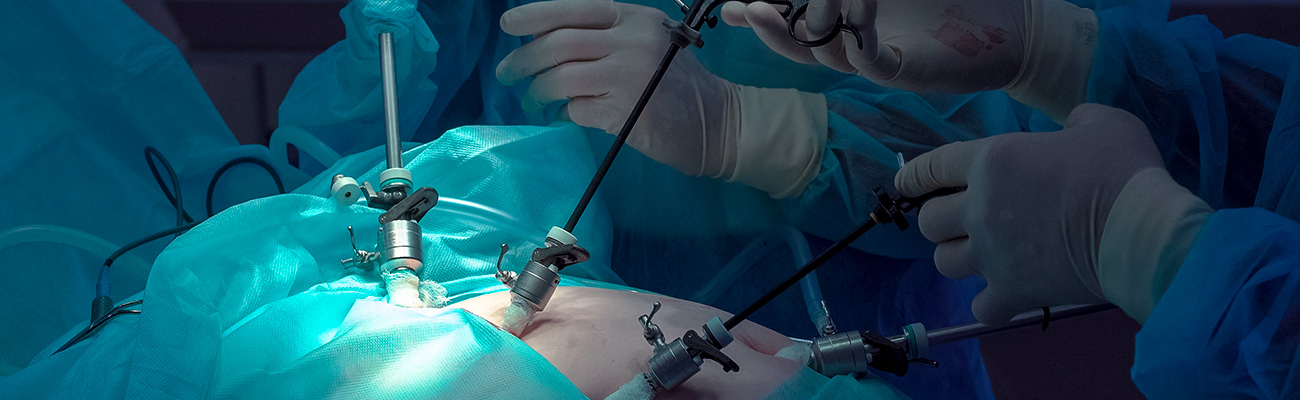
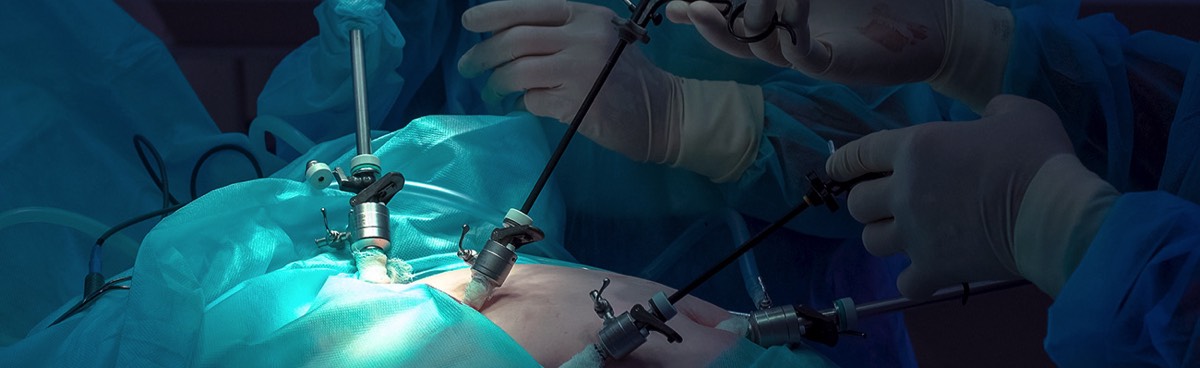
Femoral hernias may be repaired through an open or laparoscopic (keyhole) repair.
Open femoral hernia repair
The incision is at the groin crease. The hernia is identified and reduced. The hernia defect is then closed by inserting a small mesh plug that is sutured in place or simple direct sutures. The skin is then closed with absorbable suture.
Laparoscopic Totally ExtraPeritoneal (TEP) repair
Three small cuts are made in the skin above the groin.
The space behind the muscular layer (called the extraperitoneal space) is enlarged with special surgical balloons. A telescopic camera is used to visualise and locate the hernia. This is then ‘reduced’ (returned to its normal place).
A mesh is then placed to cover the hernia defect. The skin incisions are then closed with absorbable sutures.
The space behind the muscular layer (called the extraperitoneal space) is enlarged with special surgical balloons. A telescopic camera is used to visualise and locate the hernia. This is then ‘reduced’ (returned to its normal place).
A mesh is then placed to cover the hernia defect. The skin incisions are then closed with absorbable sutures.

Laparoscopic Trans Abdominal PrePeritoneal (TAPP) hernia repair
This is down within the intraperitoneal cavity (the stomach cavity).
Three incisions are made in abdominal wall above the groin crease. The peritoneum is inflated with gas. The hernia is identified and reduced (pulled back into the cavity).
An incision is made in the peritoneal sac above the hernia defect and the peritoneum is reflected (pulled away) from the overlying muscles.
The hernia defect is sutured closed and a piece of mesh is typically placed.
The peritoneum is then replaced and secured over the mesh. The skin incisions are then closed with absorbable sutures.
Three incisions are made in abdominal wall above the groin crease. The peritoneum is inflated with gas. The hernia is identified and reduced (pulled back into the cavity).
An incision is made in the peritoneal sac above the hernia defect and the peritoneum is reflected (pulled away) from the overlying muscles.
The hernia defect is sutured closed and a piece of mesh is typically placed.
The peritoneum is then replaced and secured over the mesh. The skin incisions are then closed with absorbable sutures.
Complications
Each approach has its own advantages and disadvantages, which will be discussed in detail at your consultation session. The greatest risk of undergoing hernia repair is that the hernia can come back (recurrence).
Fortunately, the recurrence rate is low with modern surgical techniques performed by experienced dedicated hernia surgeons.
Fortunately, the recurrence rate is low with modern surgical techniques performed by experienced dedicated hernia surgeons.
Postoperative care
The patient should expect to have some discomfort for one to two weeks. Therefore the patient will be discharged home with some oral pain relief. Patient is strongly encouraged to take regular pain relief in the first 7 days.
The only restriction in physical activity is not to do any heavy lifting for 3 weeks for a patient who has had an open hernia repair.
Patients who have had a laparoscopic hernia repair should not do any heavy lifting for 4 weeks. Please ask for more information.
Caution is also advised when participating in exercise.
The post-op care consultant will contact the patient 3–4 day after discharge from hospital.
The patient is typically reviewed 2–3 weeks after the operation.
Please also see: Hernia – overview
The only restriction in physical activity is not to do any heavy lifting for 3 weeks for a patient who has had an open hernia repair.
Patients who have had a laparoscopic hernia repair should not do any heavy lifting for 4 weeks. Please ask for more information.
Caution is also advised when participating in exercise.
The post-op care consultant will contact the patient 3–4 day after discharge from hospital.
The patient is typically reviewed 2–3 weeks after the operation.
Please also see: Hernia – overview
Clinical Associate Professor Hairul Ahmad
MB BS, FACEM (1999), FRACS, MS
Suite 12, Waikiki Specialist Centre,
217 Willmott Drive, Waikiki
Practice Details
Waikiki
Suite 12, Waikiki Specialist Centre,
217 Willmott Drive, Waikiki WA 6169
(08) 9592 2298
Fax: (08) 6314 1524
or email us
Office hours
9am–4pm Monday to Thursday
Affiliations



© 2024 All Rights Reserved. Content and images on this website are subject to copyright.
Email us | Sitemap | Disclaimer | Login